COMMUNICATIONS
MIKAEL GUEDJ
CYCLOSPORINE
AND MYCOPHENOLATE MOFETIL
FOR THE TREATMENT OF
BIRDSHOT CHORIORETINOPATHY
(Oral communication - ARVO May 4th 2011)
.

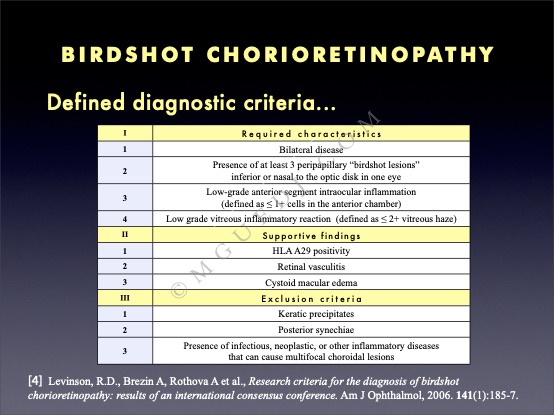









Birdshot chorioretinopathy is a disease with defined diagnostic criteria, clarified in a 2002 international consensus conference, and published in the American Journal in 2006, as summarized in the chart above.
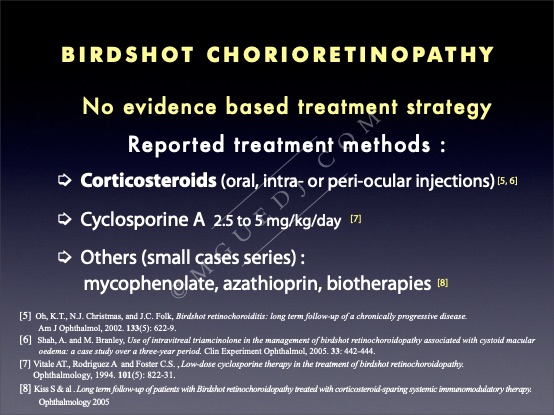
Treatments of the disease, on the other hand, are not related to any evidence based strategy. Various therapies were reported :
-
-Corticosteroids, to begin with, were the most described agents. They can be administred orally or by subtenon or intravitreal injections.
-
-Cyclosporine A at a low dose therapy had a reported effectiveness in the Vitale study.
-
-Other immunosuppressant drugs than ciclosporine were described, as mycophenolate, azathioprin or biotherapies, but only in small case series.
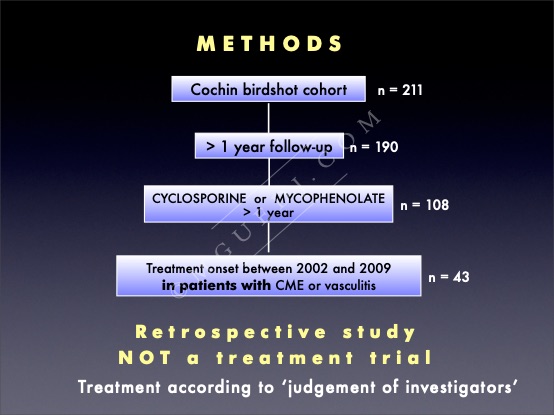
Our birdshot cohort consists of more than 200 patients, with 190 who had more than one year follow-up.
Among this group, more than 100 patients were treated by Cyclosporine or Mycophenolate. We restricted our analysis to the treatments intiated in patients with active forms on the disease, based on cystoid macular edema (CME) or vasculatis. This means we excluded patients with atrophic forms or post-inflammatory forms of the disease, and who could have recieved other immunosuppressants prior to the treatement initiation.
This was a retrospective study - not a treatment trial - and treatment was prescribed according to the judgement of investigators.
We had 43 included patients, which is a small number but quite large for this particular disease and this kind of study. We looked at the concomitant therapy these patients recieved, either corticosteroids or triamcinolone injections or none, and we more specifically analyzed 3 criteria :
-
-the oral prednisone dose
-
-the number of injections administered
-
-the proportion of macular edema and vasculitis at the one year assessment.
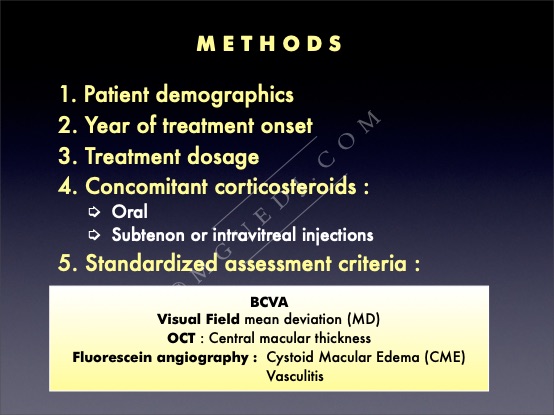
Were analyzed patient demographics, year of treatment onset, treatment dosage, concomitant corticosteroid pattern and standardized assessment criteria as described in the previous Cochin-UCLA series of papers :
-
-Functionnal criteria (best corrected visual acuity, mean deviation on visual field)
-
-Anatomical criteria (central macular thickness on OCT and CME or vasculitis on fluorescein angiography).
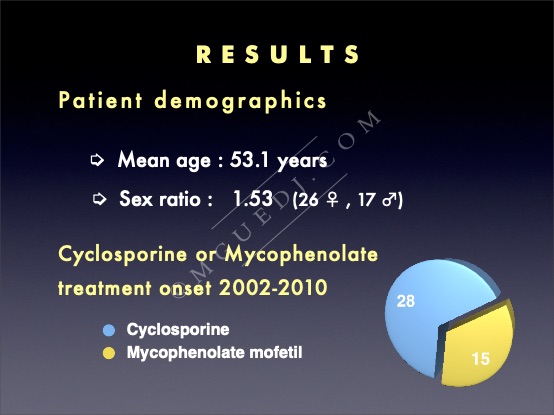
Patients mean age was 53 years, with a slight female predominance.
The number of patients was different, with more patients in the ciclosporine group.
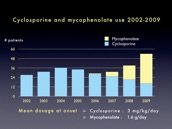
The chart below is a picture of the evolution of our practice regarding immunosuppressant use : Cyclosporine was the predominantly used drug in the beginning of the decade, until a switch around 2007-2008. Mycophenolate use began and grew from this year, to become the predominantly used drug in our patients at the end of the study.
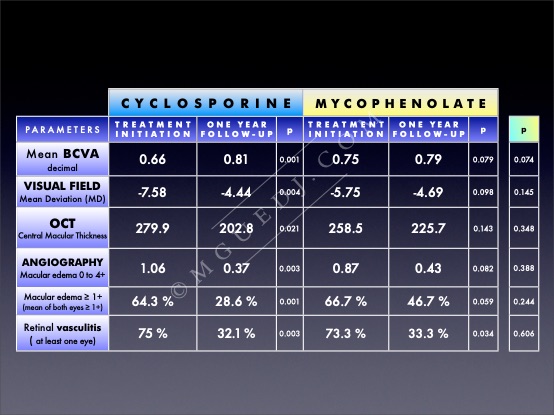
The chart above summarizes the effects of treatments :
in both groups, we observed an improvement at one year, in terms of visual acuity, visual field, macular thickness on OCT and a decrease of the proportion of patients with cystoid macular edema or vasculatis in at least one eye on fluorescein angiography.
These differences were significant in the Cyclosporine group but didn’t reach significance in the Mycophenloate group (except for retinal vasculitis), probably due to a fewer number of patients.
In addition, when it comes to comparison between Cyclosporine and Mycophenolate groups, we found no difference of effectiveness for any of these parameters, regarding both groups.
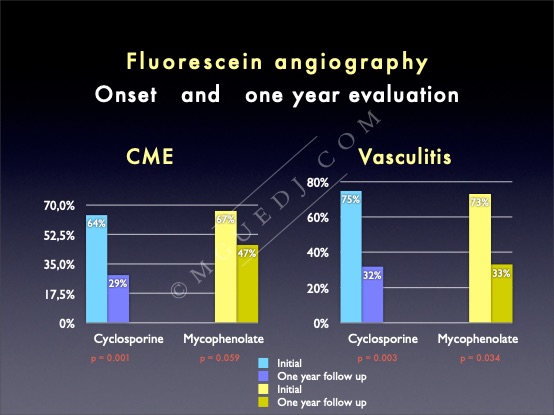
The graphs below show that the proprotion of patients with cystoid macular edema or vasculitis were comparable in both groups at onset, and that both groups had decreasing CME. However, there’s a slightly greater percentage of decreasing CME in the Cyclosporine than the Mycophenloate group, although this difference didn’t reach stastistical significance.
Regarding vasculitis, we found the same percentage of decreasing vasculitis at the one year evaluation in both groups.
This is the case of one of our patients treated with Cyclosporine 3 mg/kg/day and oral prednisone 0.5 mg/kg/day, with a macular edema both seen on OCT and on FA. The improvement is visible with a decrease of the CME and the OCT going back to normal at the one year assessment, with a slow tapering off prednisone, reaching 5 mg per day at this level.
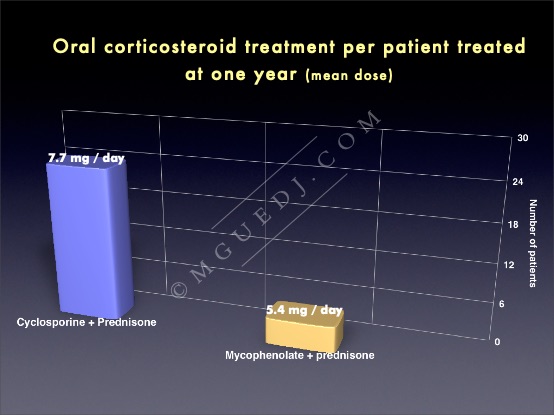
This was the unexpected result from our study : when we retrospectively analyzed our corticosteroid treatment pattern, we realized that, back in 2002, when Cyclosporine was the immunosuppressant of choice (or ‘weapon of choice’ as would have said Fatboy Slim) for our patients, oral corticosteroids were systematically used at the same time, whereas later in the decade, not all of our patients treated by Mycophenolate had concomitant oral prednisone, and actually only a minority (one third of these patients) were treated at the same time with oral corticosteroids.
Even in the cases where corticosteroids were initiated together with Mycophenolate, smaller dose of oral prednisone remained after one year.
What had happened was that in the mean time, local corticosteroid injections had taken an increasing par of the treatment strategy, and we observed a greater number of injections per patient had been used in the Mycophenolate treated group. And this complicated the retrospective interpretation of results for the comparison between the Mycophenolate and Cyclosporine groups.
This is the example of a 72 year old birdshot patient with a CME, that shows the dramatic effect of one triamcinolone injection on the macular thickness and the visual acuity, increasing from counting fingers to 20/200 one month after the injection.
It is now clear that assessment of patients with birdshot chorioretinopathy is a complex task : it’s along term disease, with heterogeneous presentation and multiple outcome measures or treatment strategies. For these reasons, the Cochin-UCLA approach is based on a yearly standardized assessment, with criteria both anatomical and functionnal. Our analysis restricted to forms with CME or vasculitis, and to two immunosuppressants, Cyclosporine and Mycophenolate.
There are numerous limitations to our study. It is once again a retrospective analysis, with a different number of patients because Cyclosporine has been around for a longer time than Mycophenolate, which is also the reason why we chose an assessment of treatment after one year only.
Concomitant therapies were uncontrolled, and systemic effects of drugs were analyzed in a separate study.
The comparison of the two groups found no difference in population at baseline (same age, same proportion of CME and vasculitis), and at the one year assessment, no differential effect was recorded in terms of visual acuity, cystoid macular edema and vasculitis.
We observed a variable pattern of corticosteroid use, with more oral corticosteroids in the earlier study period, and more intra or periocular injections in the later study period.
Taking into account all the limitations of our study, we observed comparable outcomes with both treatment methods, and an evolution of treatment practices. Treatment trials remain needed to gather evidence based data.